University of Illinois at Chicago
|
The goal of this project was to conduct an evaluation of the work developed by the Principal Investigator and colleagues at the University of Illinois at Chicago (UIC) in developing and implementing interprofessional education aimed at preparing health professions students to address health disparities. Using a cross sectional study design, we explored the perspectives of faculty and staff responsible for curriculum planning across three UIC regional campuses through an online survey designed to map interprofessional learning experiences. The results of the survey indicate a considerable number of educational offerings utilizing interprofessional teaching and learning. While mapping health disparities training was the primary focus of this study, our findings highlight the breadth of IPE learning experiences that are currently offered at UIC.
impact
|
Created "Interprofessional Approaches to Health Disparities" course and other IPE courses serving 3,000+ health professions students per year. |
Established 30-member IPE task force and completed strategic planning for IPE. Strengthened collaborations among UI healthcare system and health sciences colleges. |
APTR Project proposal for 2007/2008 ipe institute
|
Our initial IPE Institute Project was titled: "Interprofessional Reflective Practice to Address Health Needs of Vulnerable Patients." The context and rationale for this learning experience was based on the need for interprofessional teamwork as an essential factor for effective delivery of health care to all patients, particularly the vulnerable and underserved.
|
Sustained the post-institute IPE activity or project after the initial year of implementation: Yes, but with major modifications |
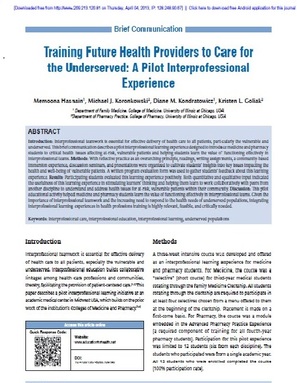
Our pilot interprofessional learning experience was designed to introduce medicine and pharmacy students to critical health issues affecting at-risk, vulnerable patients and helping students learn the value of functioning effectively in interprofessional teams. We embedded the pilot IPE experience within our longitudinal Patient-centered Medicine Scholars Program. With reflective practice as an overarching principle, readings, writing assignments, a community-based immersion experience, discussion seminars and presentations were organized to cultivate students’ insights into key issues impacting the health and well-being of vulnerable patients. A written program evaluation form was used to gather students’ feedback about this learning experience. Participating students evaluated this learning experience positively. Both quantitative and qualitative input indicated the usefulness of this learning experience in stimulating learners’ thinking and helping them learn to work collaboratively with peers from another discipline to assess and address health issues for at-risk, vulnerable patients within their community. Based on participants feedback, this pilot educational activity helped medicine and pharmacy students learn the value of functioning effectively in interprofessional teams. This pilot work was the forerunner to our IPE-based additional program development at UIC. Given the importance of interprofessional teamwork and the increasing need to respond to the health needs of underserved populations, integrating interprofessional learning experiences in health professions training is highly relevant, feasible and critically needed.
Our pilot interprofessional learning experience was designed to introduce medicine and pharmacy students to critical health issues affecting at-risk, vulnerable patients and helping students learn the value of functioning effectively in interprofessional teams. We embedded the pilot IPE experience within our longitudinal Patient-centered Medicine Scholars Program. With reflective practice as an overarching principle, readings, writing assignments, a community-based immersion experience, discussion seminars and presentations were organized to cultivate students’ insights into key issues impacting the health and well-being of vulnerable patients. A written program evaluation form was used to gather students’ feedback about this learning experience. Participating students evaluated this learning experience positively. Both quantitative and qualitative input indicated the usefulness of this learning experience in stimulating learners’ thinking and helping them learn to work collaboratively with peers from another discipline to assess and address health issues for at-risk, vulnerable patients within their community. Based on participants feedback, this pilot educational activity helped medicine and pharmacy students learn the value of functioning effectively in interprofessional teams. This pilot work was the forerunner to our IPE-based additional program development at UIC. Given the importance of interprofessional teamwork and the increasing need to respond to the health needs of underserved populations, integrating interprofessional learning experiences in health professions training is highly relevant, feasible and critically needed.
Current ipe activity/project description
In 2013, the Principal Investigator, Dr. Hasnain, received the prestigious Macy Faculty Award from the Josiah Macy Jr. Foundation. This award is given to select educators nationally to accelerate needed reforms in health professions education to accommodate the dramatic changes occurring in medical practice and health care delivery. For her Macy award project, Dr. Hasnain led the development and implementation of “Interprofessional Approaches to Health Disparities (IAHD)” a longitudinal interprofessional course offered during the Fall and Spring semesters for health professions students at UIC. The goal of this program is to equip learners with essential skills to improve health care for underserved populations and transform health disparities through interprofessional education, research and collaborative practice.
Dr. Hasnain and her colleagues successfully designed, developed and launched the new IAHD course. This involved substantial groundwork including getting engagement from the leadership of various health professions colleges at UIC; establishing a team of interprofessional faculty colleagues who served as course faculty; developing a sound curriculum; and, recruiting learners. Twenty-eight students from medicine, nursing, pharmacy and public health participated in the inaugural program year, working in five focus areas: Domestic Violence, Geriatrics, HIV/AIDS, Homelessness, and Immigrant & Refugee Health. Student teams engaged in didactic and experiential learning activities, including mentored community-based participatory research (CBPR) and quality improvement (QI) projects. A substantial element of learning included training in CBPR methodology and hands on work with vulnerable persons and staff at community agencies. All student teams developed and carried out CBPR projects (project abstracts available upon request). Program evaluation indicates that learners viewed the learning experience positively. Learners also provided constructive feedback for strengthening the program. An important lesson from this experience is the reminder that designing and implementing interprofessional education is not an easy task. Dr. Hasnain remains optimistic that this project will lead to meaningful contributions to advancing the health professions education science towards discovering new, collaborative models for training future healthcare workforce, to better assess and address the needs of our evolving patient populations through engaging both a broad interprofessional team as well as patient groups to reduce health disparities.
Our programmatic competencies related to interprofessional collaboration encompass the domains of values and ethics, roles and responsibilities, interprofessional communication, and teams and teamwork. These four competency domains were initially proposed by the Interprofessional Education Collaborative (IPEC) in 2011. In the time since the IPEC 2011 publication, it has become clear that interprofessional collaboration stands as a domain unto itself (IPEC, 2016). Furthermore, creating shared taxonomy among the health professions can serve to streamline and synergize educational activities and related assessment and evaluation efforts. Our longer term goal is to broaden the interprofessional competencies to better achieve the Triple Aim (improve the patient experience of care, improve the health of populations, and reduce the per capita cost of health care), with particular reference to population health.
At the institutional level, a group of faculty leaders interested in developing IPE initiatives at UIC has been working steadily over the last several years. The impetus for this work is based on the rationale that health professions education and practice tend to occur in silos resulting in suboptimal teamwork that is a missed opportunity not only health professional students’ professional development in their formative years but also for improving patient outcomes and reducing unnecessary costs to the health care system. UIC has seven health colleges and over 5000 students enrolled in health professions education programs. Early IPE efforts at UIC were fragmented and developing in silos. As awareness of IPE grew, the faculty coalesced to approach the UIC administration to create centralized efforts with institutional support. Subsequently, after concerted effort, a strategic plan was developed in 2015 with input from a wide variety of stakeholders. As part of the strategic plan, an IPE Directorship was established within the Office of the Vice Chancellor for Health Affairs with responsibility for the comprehensive and integrated development of IPE initiatives. A critical component in the institutional support was the development of a transformative model of interprofessional education and collaborative practice. This model includes the University of Illinois healthcare system and the UIC health science colleges as committed partners in the development of IPE efforts.
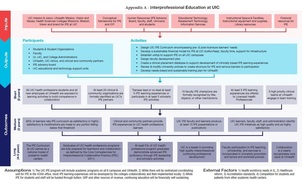
A rigorous process was used to develop a robust framework that took into account the structural, human, political and symbolic dimensions. Over a period of a year, a 30-member IPE task force carried out an in-depth SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis, environmental scan, and conducted stakeholder interviews to develop a strategic plan to be implemented over the next 3-5 years. Please see Appendix A - UIC IPE Logic Model.
Dr. Hasnain and her colleagues successfully designed, developed and launched the new IAHD course. This involved substantial groundwork including getting engagement from the leadership of various health professions colleges at UIC; establishing a team of interprofessional faculty colleagues who served as course faculty; developing a sound curriculum; and, recruiting learners. Twenty-eight students from medicine, nursing, pharmacy and public health participated in the inaugural program year, working in five focus areas: Domestic Violence, Geriatrics, HIV/AIDS, Homelessness, and Immigrant & Refugee Health. Student teams engaged in didactic and experiential learning activities, including mentored community-based participatory research (CBPR) and quality improvement (QI) projects. A substantial element of learning included training in CBPR methodology and hands on work with vulnerable persons and staff at community agencies. All student teams developed and carried out CBPR projects (project abstracts available upon request). Program evaluation indicates that learners viewed the learning experience positively. Learners also provided constructive feedback for strengthening the program. An important lesson from this experience is the reminder that designing and implementing interprofessional education is not an easy task. Dr. Hasnain remains optimistic that this project will lead to meaningful contributions to advancing the health professions education science towards discovering new, collaborative models for training future healthcare workforce, to better assess and address the needs of our evolving patient populations through engaging both a broad interprofessional team as well as patient groups to reduce health disparities.
Our programmatic competencies related to interprofessional collaboration encompass the domains of values and ethics, roles and responsibilities, interprofessional communication, and teams and teamwork. These four competency domains were initially proposed by the Interprofessional Education Collaborative (IPEC) in 2011. In the time since the IPEC 2011 publication, it has become clear that interprofessional collaboration stands as a domain unto itself (IPEC, 2016). Furthermore, creating shared taxonomy among the health professions can serve to streamline and synergize educational activities and related assessment and evaluation efforts. Our longer term goal is to broaden the interprofessional competencies to better achieve the Triple Aim (improve the patient experience of care, improve the health of populations, and reduce the per capita cost of health care), with particular reference to population health.
At the institutional level, a group of faculty leaders interested in developing IPE initiatives at UIC has been working steadily over the last several years. The impetus for this work is based on the rationale that health professions education and practice tend to occur in silos resulting in suboptimal teamwork that is a missed opportunity not only health professional students’ professional development in their formative years but also for improving patient outcomes and reducing unnecessary costs to the health care system. UIC has seven health colleges and over 5000 students enrolled in health professions education programs. Early IPE efforts at UIC were fragmented and developing in silos. As awareness of IPE grew, the faculty coalesced to approach the UIC administration to create centralized efforts with institutional support. Subsequently, after concerted effort, a strategic plan was developed in 2015 with input from a wide variety of stakeholders. As part of the strategic plan, an IPE Directorship was established within the Office of the Vice Chancellor for Health Affairs with responsibility for the comprehensive and integrated development of IPE initiatives. A critical component in the institutional support was the development of a transformative model of interprofessional education and collaborative practice. This model includes the University of Illinois healthcare system and the UIC health science colleges as committed partners in the development of IPE efforts.
A rigorous process was used to develop a robust framework that took into account the structural, human, political and symbolic dimensions. Over a period of a year, a 30-member IPE task force carried out an in-depth SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis, environmental scan, and conducted stakeholder interviews to develop a strategic plan to be implemented over the next 3-5 years. Please see Appendix A - UIC IPE Logic Model.
|
IPE OFFERINGS INCLUDE:
Do you have formal affiliation agreements with any of the schools mentioned above?
All health professions schools involved are part of the IPE strategic planning taskforce. |
PROFESSIONS/DISCIPLINES/SCHOOLS INVOLVED:
BS in Health Information Management or MS/certificate in Health Informatics BS in Nursing BS or MS in Nutrition Doctor of Dental Medicine or Dental Surgery Doctor of Medicine Doctor of Pharmacy Doctor of Physical Therapy Master of Health Administration Master of Science in Nursing (APN) Master of Science in Nursing (GEP) Master of Public Health Master of Social Work MS or Doctorate in Occupational Therapy or Occupational Therapy |
ACADEMIC LEVELS TARGETED:
- Undergraduate
- Graduate
- Professional Other: Clinical Trainees - Residents and Fellows
COURSE DESCRIPTION:
Number of students enrolled in IPE course during the most recent academic year:
There are a number of courses and other learning experiences related to IPE that are currently offered to all UIC students. Please see Appendix B – College Enrollment.
Is this a shared/cross-listed course? Yes
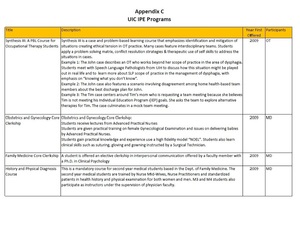
Title of Course(s): Please see Appendix C – UIC IPE Programs
Number of students enrolled in IPE course during the most recent academic year:
There are a number of courses and other learning experiences related to IPE that are currently offered to all UIC students. Please see Appendix B – College Enrollment.
Is this a shared/cross-listed course? Yes
Title of Course(s): Please see Appendix C – UIC IPE Programs
|
PLACEMENT SITES FOR ANY SERVICE-LEARNING COMPONENTS:
|
EVALUATION METHODS USED FOR THE SUBGRANT PROJECT:
|
lessons /results/outcomes
Lessons Learned:
There are several lessons we have learned through our journey of program development and implementation. Below are some key lessons we continue to pay heed to as we proceed.
There are several lessons we have learned through our journey of program development and implementation. Below are some key lessons we continue to pay heed to as we proceed.
- When people start working individually and in silos, there is a lot of wasted energy and resources. Hence, it is critically important to get people engaged early on to work together collaboratively.
- Theory and evidence need to be integrated in curriculum transformation efforts. We have drawn heavily from theoretical and conceptual frameworks, such as Kotter’s principles of change management and Kern’s principles of curriculum development. We use these as conceptual frameworks and core foundation for developing IPE at our institution.
- Curriculum development should be responsive to local, regional and national trends and emerging needs in health professions education and health care delivery and practice.
- Involving student input is essential in developing learner-centered and meaningful educational programs.
- The “interprofessionalism” of any IPE program includes faculty as well as students. Recruitment and development of an interprofessional faculty group improves the likelihood of program sustainability as well as acting as an impetus for other collaborative IPE projects. Proactive recruitment and faculty development efforts are necessary to ensure widespread participation in interprofessional activities.
- Scholarly work must be central to program development and should be made a priority.
- Institutional support is crucial in providing the necessary infrastructure and support for program development, growth and sustainability.
- Successful teams thrive when there is trust, respect and shared goals and values. Our IPE team has been successful in collaborative program development, scholarship (papers, presentations), obtaining grant funding, and developing a network of mutually-supportive colleagues and friends.
- Finally, developing anything that is complex and multilayered can be both an exhilarating and exasperating experience. This is certainly true of curriculum development and charting into new territory, such as interprofessional education. Remembering what a great privilege it is to be a part of positively influencing the learning of our future health professionals is an ongoing extrinsic motivator for our team; when you do something with love, joy and gratitude it is so much better!
Publications:
Hasnain M, Koronkowski MJ, Kondratowicz DM, Goliak KL. Training future health providers to care for the underserved: a pilot interprofessional experience. Educ Health (Abingdon). 2012 Sep-Dec;25(3):204-7. doi: 10.4103/1357-6283.109790.
PubMed PMID: 23823641.
Hasnain M, Schwartz A, Girotti J, Bixby A, Rivera L; UIC Experiences of Care Project Group. Differences in patient-reported experiences of care by race and acculturation status. J Immigr Minor Health. 2013 Jun;15(3):517-24. doi: 10.1007/s10903-012-9728-x. PubMed PMID: 23054545.
Hasnain M, Massengale L, Dykens A, Figueroa E. Health disparities training in residency programs in the United States. Fam Med. 2014 Mar;46(3):186-91. Review. PubMed PMID: 24652636.
Hasnain M, Gruss V, Keehn M, Peterson E, Valenta AL, Kottorp A. Development and validation of a tool to assess self-efficacy for competence in interprofessional collaborative practice. J Interprof Care. 2017 Mar;31(2):255-262. doi: 10.1080/13561820.2016.1249789. Epub 2017 Jan 27.
Hasnain M, Koronkowski MJ, Kondratowicz DM, Goliak KL. Training future health providers to care for the underserved: a pilot interprofessional experience. Educ Health (Abingdon). 2012 Sep-Dec;25(3):204-7. doi: 10.4103/1357-6283.109790.
PubMed PMID: 23823641.
Hasnain M, Schwartz A, Girotti J, Bixby A, Rivera L; UIC Experiences of Care Project Group. Differences in patient-reported experiences of care by race and acculturation status. J Immigr Minor Health. 2013 Jun;15(3):517-24. doi: 10.1007/s10903-012-9728-x. PubMed PMID: 23054545.
Hasnain M, Massengale L, Dykens A, Figueroa E. Health disparities training in residency programs in the United States. Fam Med. 2014 Mar;46(3):186-91. Review. PubMed PMID: 24652636.
Hasnain M, Gruss V, Keehn M, Peterson E, Valenta AL, Kottorp A. Development and validation of a tool to assess self-efficacy for competence in interprofessional collaborative practice. J Interprof Care. 2017 Mar;31(2):255-262. doi: 10.1080/13561820.2016.1249789. Epub 2017 Jan 27.