MCPHS University
|
IMPACT
|
IPE events serve up to 600 students per year and involve 77 faculty members. |
Developed partnerships with community health centers, hospitals, and retirement communities. |
AptR project proposal for 2007/2008 ipe institute
|
Despite barriers such as scheduling conflicts and various educational experiences, this course enabled students to gain greater respect for the contributions of other professions and made them more patient-centered. Also, interprofessional student teams positively influenced the health attitudes and behaviors of the elders whom they encountered.
|
Sustained the post-institute IPE activity or project after the initial year of implementation: No, but alternative IPE programs were developed soon after |
Recognizing the importance of interprofessional education (IPE), we developed a pilot IPE course at our institution that included a total of ten Nursing, BS Health Psychology, Pre-medical, and Pharmacy students. Course goals were for students to (1) learn about, practice, and enhance their skills as members of an interprofessional team; and (2) create and deliver a community-based service learning program to help prevent or slow the progression of cardiovascular disease in elders. Teaching methods included lecture, role play, case studies, peer editing, oral and poster presentation, and discussion. Interprofessional student teams created and delivered two different health promotion programs at a senior care facility.
current ipe activity/project description
Numerous interprofessional education initiatives have been developed at MCPHS since 2009, primarily in academic programs in which IPE is required to be included in the curriculum, i.e. Pharmacy, Nursing, Dental Hygiene, Physical Therapy, Public Health and Medical Education. The following outlines the structural, human resource, political and symbolic dimensions of IPE at MCPHS, 2009-2016.
Structural Dimensions:
- In 2014, MCPHS developed its first Strategic IPE Plan to define core competencies and effectively prepare students.
- A symposium was held for all faculty in May, 2014 to outline a plan to guide development of an IPE curriculum for the University. Outcomes from this IPE Symposium included:
- Development of Plexus Mission Statement
- Adoption of Core Competency Domains
- Establishment of Organization and Leadership unit within the Provost’s Office
- Establishment of IPE working Group
- Initiation of Policy to offer IPE Match-Grants
- IPE’s primary goal:
- Promote IPE Core Competencies related to values/ethics; roles/responsibilities; interprofessional communication; teams and teamwork.
- Three secondary goals were established to support this primary goal:
- Engage Faculty
- Build partnerships between schools with MCPHS University and with community partners
- Prepare students utilizing active learning, classroom and clinical experiences, and solid assessment
Human Dimensions:
Our current IPE review indicates that faculty readiness to incorporate IPE activities into the curriculum is varied. Seventy-seven of 600 faculty (~13%) reported on IPE activities in response to our survey. All schools within the university were represented, with no significant difference. Assistant Professors are most involved in IPE, with decreasing engagement with increasing rank. Collectively, 24% of faculty reported that they are planning additional IPE activities. The primary reason for not continuing IPE was reported to be time constraints and other logistical issues.
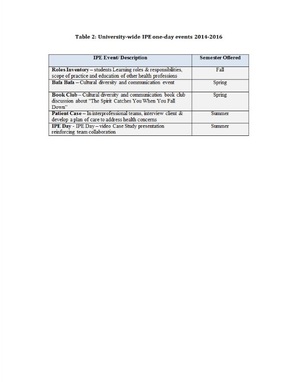
A faculty-developed IPE Working Group has sponsored the largest IPE events on two MCPHS campuses during the past three years. Table 2: University-wide IPE one-day events 2014-2016 (see Resources)
Faculty may apply to MCPHS for small grants to assist in the development and implementation of faculty-initiated IPE projects.
Our current IPE review indicates that faculty readiness to incorporate IPE activities into the curriculum is varied. Seventy-seven of 600 faculty (~13%) reported on IPE activities in response to our survey. All schools within the university were represented, with no significant difference. Assistant Professors are most involved in IPE, with decreasing engagement with increasing rank. Collectively, 24% of faculty reported that they are planning additional IPE activities. The primary reason for not continuing IPE was reported to be time constraints and other logistical issues.
A faculty-developed IPE Working Group has sponsored the largest IPE events on two MCPHS campuses during the past three years. Table 2: University-wide IPE one-day events 2014-2016 (see Resources)
Faculty may apply to MCPHS for small grants to assist in the development and implementation of faculty-initiated IPE projects.
Political Dimensions:
IPE is currently still promoted by individual faculty and faculty groups (e.g., IPE Working Group), who have integrated IPE objectives into existing courses or sponsored campus-wide IPE events. MCPHS leadership is supportive of such initiatives.
While the Strategic IPE Plan was established in 2014, and the university is currently seeking a replacement for the position of IPE Director to oversee IPE programming.
Allocated resources for IPE include small university grants available to faculty who propose and receive approval for IPE projects. Faculty may apply to MCPHS for small grants to assist in the development and implementation of faculty-initiated IPE projects.
IPE is currently still promoted by individual faculty and faculty groups (e.g., IPE Working Group), who have integrated IPE objectives into existing courses or sponsored campus-wide IPE events. MCPHS leadership is supportive of such initiatives.
While the Strategic IPE Plan was established in 2014, and the university is currently seeking a replacement for the position of IPE Director to oversee IPE programming.
Allocated resources for IPE include small university grants available to faculty who propose and receive approval for IPE projects. Faculty may apply to MCPHS for small grants to assist in the development and implementation of faculty-initiated IPE projects.
Symbolic Dimensions:
Currently, results suggest that there is a lack of clarity and understanding regarding the definition of IPE at MCPHS. For example, variation in program descriptions suggested some programs are interdisciplinary rather than interprofessional.
Also, a review of the course syllabi and curriculum for Pharmacy, Physical Therapy, Physician Assistant Studies, Nursing, Optometry professional programs (C. Babin, Interprofessional Education Curriculum Audit Across Graduate Healthcare Programs, Spring 2016) indicated inconsistencies in IPE learning objectives among these programs. Also, while these five programs require their students to have experiential learning/clinical/field placements as part of their curriculum as well as IPE learning experiences, students function under the direction of their discipline-specific clinical instructors at clinical settings, and IPE learning objectives/experiences are not clear in these settings.
Currently, results suggest that there is a lack of clarity and understanding regarding the definition of IPE at MCPHS. For example, variation in program descriptions suggested some programs are interdisciplinary rather than interprofessional.
Also, a review of the course syllabi and curriculum for Pharmacy, Physical Therapy, Physician Assistant Studies, Nursing, Optometry professional programs (C. Babin, Interprofessional Education Curriculum Audit Across Graduate Healthcare Programs, Spring 2016) indicated inconsistencies in IPE learning objectives among these programs. Also, while these five programs require their students to have experiential learning/clinical/field placements as part of their curriculum as well as IPE learning experiences, students function under the direction of their discipline-specific clinical instructors at clinical settings, and IPE learning objectives/experiences are not clear in these settings.
IPE OFFERINGS INCLUDE:
- IPE Courses (integration into existing courses; no separate specific IPE courses)
- IPE Clinical Rotations or Clerkships (varied – IPE not clearly articulated)
- IPE Senior Projects/Capstones
- IPE Community Projects/ Service Learning
- IPE Extra-Curricular Activities
- Other: Online learning opportunities; IPE Days: large one-day events (200-600-students)
|
PROFESSIONS/DISCIPLINES/SCHOOLS INVOLVED:
|
FORMAL AFFILIATION AGREEMENTS WITH ANY OF THE SCHOOLS MENTIONED ABOVE:
These are all within MCPHS University. ACADEMIC LEVELS TARGETED:
|
COURSE DESCRIPTION:
No stand-alone IPE courses are offered at MCPHS. MCPHS faculty either integrate IPE experiences into existing courses, or provide single IPE events that engage 200-600 students from the professional programs of Pharmacy, Physical Therapy, Physician Assistant Studies, Dental Hygiene, Nursing, and Optometry.
No stand-alone IPE courses are offered at MCPHS. MCPHS faculty either integrate IPE experiences into existing courses, or provide single IPE events that engage 200-600 students from the professional programs of Pharmacy, Physical Therapy, Physician Assistant Studies, Dental Hygiene, Nursing, and Optometry.
PLACEMENT SITES FOR ANY SERVICE-LEARNING COMPONENTS:
- Community Health Centers
- Hospitals (clinical rotations/field placements)
- Other Nonprofit Human Service Agencies (retirement communities)
lessons/results/outcomes
Evaluation Results:
Follow-up to this subgrant evaluation includes development of a task force to:
Data Outcomes
126 faculty (21%) responded to the survey. 77 faculty reported IPE engagement, and they provided 57 program descriptions. There was no significant difference (p=0.062) in MCPHS school representation. Junior faculty reported significantly higher IPE engagement (p=0.002). Descriptive statistics indicated: 52% involved at least five faculty; 53% took place in traditional classroom settings; 52% occurred since 2014; 47% were less than half a semester; 58% address professional accreditation requirements; inclusion of prevention and population health topics is highly variable; and only 24% are planning additional activities. Barriers included time constraints, perceived minimal administrative support and logistical challenges of organization and collaboration.
Conclusions
Quantitative data analysis indicated an increase in IPE engagement since 2009; however, only one-fourth of involved faculty reported intentions to plan additional activities. There is a lack of clarity and understanding regarding the definition of IPE, suggested by the variation in program descriptions. Prevention and population health topics were not consistently included and some faculty indicated uncertainty regarding the content of such topics.
As junior faculty are the most involved in IPE activities but with limited intentions to continue, there is an institutional opportunity for senior faculty to mentor and model IPE engagement, with a focus on prevention and population health. Suggested next steps include the development of a task force to: disseminate standard IPE definitions and competencies; assess MCPHS using the Interprofessional Education Assessment and Planning Instrument for Academic Institutions (Greer & Clay, 2010); and collaborate with other health professions institutions.
- Quantitative data analysis indicated an increase in IPE engagement since 2009;
- Junior faculty are the most involved in IPE activities.
- Only one-fourth of current IPE faculty intend to engage in additional activities;
- There is a lack of clarity and understanding regarding the definition of IPE;
- Variation in program descriptions suggested some programs are interdisciplinary rather than interprofessional;
- Most IPE programming takes place in traditional classroom setting rather than clinical sites;
- Prevention and population health topics were not consistently included and some faculty indicated uncertainty regarding such topics;
Follow-up to this subgrant evaluation includes development of a task force to:
- Continue self-study reports from schools that require IPE in their accreditation criteria;
- Conduct in-depth interviews with current IPE participants;
- Disseminate standard IPE definitions and competencies;
- Assess MCPHS using the IPE Assessment and Planning Instrument for Academic Institutions (Greer & Clay, 2010);
- Provide support and encourage more inclusion of prevention and population health topics;
- Provide opportunities for senior faculty to mentor and model IPE engagement;
- Add specific IPE objectives to the appropriate course syllabi in each program that has IPE accreditation requirements;
- Incorporate IPE more systematically into the multiple pre-professional undergraduate programs at MCPHS;
- Collaborate with other health professions involved in IPE, through APTR and other organizations.
Data Outcomes
126 faculty (21%) responded to the survey. 77 faculty reported IPE engagement, and they provided 57 program descriptions. There was no significant difference (p=0.062) in MCPHS school representation. Junior faculty reported significantly higher IPE engagement (p=0.002). Descriptive statistics indicated: 52% involved at least five faculty; 53% took place in traditional classroom settings; 52% occurred since 2014; 47% were less than half a semester; 58% address professional accreditation requirements; inclusion of prevention and population health topics is highly variable; and only 24% are planning additional activities. Barriers included time constraints, perceived minimal administrative support and logistical challenges of organization and collaboration.
Conclusions
Quantitative data analysis indicated an increase in IPE engagement since 2009; however, only one-fourth of involved faculty reported intentions to plan additional activities. There is a lack of clarity and understanding regarding the definition of IPE, suggested by the variation in program descriptions. Prevention and population health topics were not consistently included and some faculty indicated uncertainty regarding the content of such topics.
As junior faculty are the most involved in IPE activities but with limited intentions to continue, there is an institutional opportunity for senior faculty to mentor and model IPE engagement, with a focus on prevention and population health. Suggested next steps include the development of a task force to: disseminate standard IPE definitions and competencies; assess MCPHS using the Interprofessional Education Assessment and Planning Instrument for Academic Institutions (Greer & Clay, 2010); and collaborate with other health professions institutions.