Following an interprofessional education retreat, Albert Einstein College of Medicine’s (Einstein) family medicine clerkship built on an existing team-based learning (TBL) experience and prior relationship with the Columbia University School of Nursing (Columbia) family nurse practitioner program for an interprofessional education initiative. Four mixed teams worked at Einstein weekly for 3 two-hour TBL sessions on preventive health and chronic disease management topics, supervised by family medicine faculty. The initiative includes over 180 Einstein and 90 Columbia students per academic year.
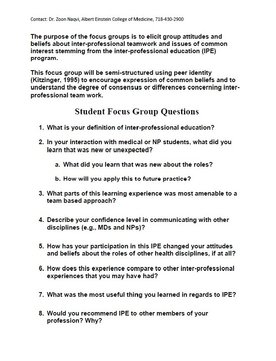
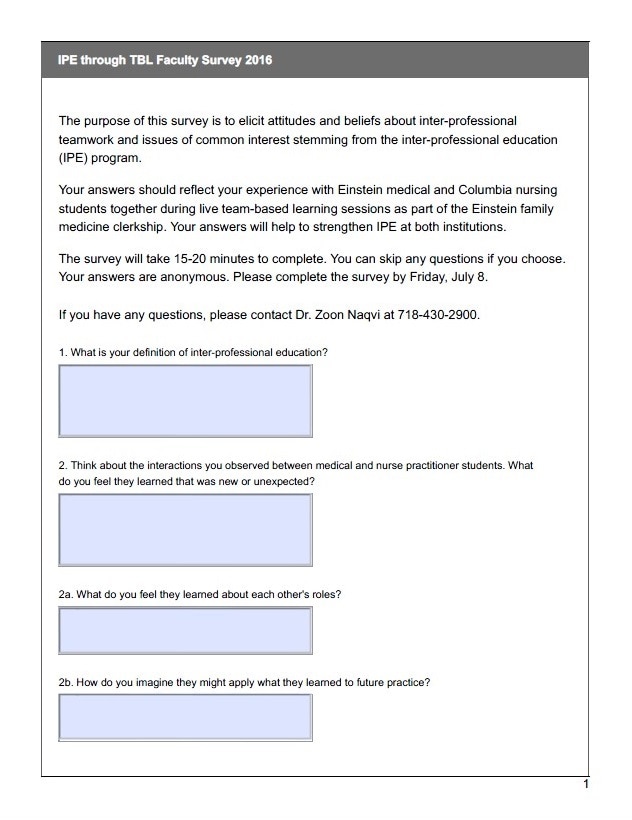
METHODS: Our goal was to analyze student attitudes regarding interprofessional teamwork in a joint in-person TBL experience. Our objectives included: (a) improving attitudes on interprofessional teamwork pre- vs. post-experience by 10% using a validated scale (Interprofessional Attitude Scale, IPAS); and (b) clarifying aspects of the training experience that promoted or hindered interprofessional teamwork. We compared pre- and post-test averages for the 5 subdomains for all students and each profession, using a two-tailed t-test. We qualitatively assessed barriers to and facilitators of this experience to learning about interprofessional teamwork through focus groups with 16 Einstein and 5 Columbia students, plus an open-ended survey including 4 Einstein and 1 Columbia faculty members, all analyzed thematically.
METHODS: Our goal was to analyze student attitudes regarding interprofessional teamwork in a joint in-person TBL experience. Our objectives included: (a) improving attitudes on interprofessional teamwork pre- vs. post-experience by 10% using a validated scale (Interprofessional Attitude Scale, IPAS); and (b) clarifying aspects of the training experience that promoted or hindered interprofessional teamwork. We compared pre- and post-test averages for the 5 subdomains for all students and each profession, using a two-tailed t-test. We qualitatively assessed barriers to and facilitators of this experience to learning about interprofessional teamwork through focus groups with 16 Einstein and 5 Columbia students, plus an open-ended survey including 4 Einstein and 1 Columbia faculty members, all analyzed thematically.
Impact
|
Team-based learning for 190 medical students and 90 nursing students per year. |
Developed collaboration between Albert Einstein College of Medicine and Columbia University School of Nursing. |
APTR PROJECT PROPOSAL FOR 2007/2008 IPE INSTITUTE
|
The project created a course on applied public health strategies to address the obesity epidemic, bringing together faculty from a number of professions across Yeshiva University (and outside guests). The course went well, and the inclusion of a hands-on group project was particularly effective. However, scheduling conflicts depressed course registration, and the plan to transition the course into the new MPH program foundered when the MPH program closed due to lack of funds.
|
Sustained the post-institute IPE activity or project after the initial year of implementation: - No, current IPE initiatives began more than 2 years after the Institute - The institute project concluded in 2012 - The current project began in 2014 |
CURRENT IPE ACTIVITY/PROJECT DESCRIPTION
The purpose of our interprofessional prevention education (IPPE) program is to foster positive attitudes around interprofessional teamwork, knowledge of one’s own and other professionals’ roles on the team, and skills in developing solutions based on team dynamics. Our specific objectives include:
This program built on a recently developed new competency framework for the medical school, and hoped to respond to evolving accreditations standards around interprofessional education. The program aimed to generate productive learning experiences that could, in addition to transmitting traditional knowledge, provide team activities that shift attitudes, particularly in the domains of: (1) teamwork, roles, and responsibilities; and (2) interprofessional biases. The ultimate goal was to deliver an educational experience that supports provision of patient-, family-, and community-centered care that improves meaningful patient outcomes.
This was the first truly interprofessional learning experience for either training program. While it is sustainable, it fell short of its goals and objectives in key respects. Nevertheless, it created a framework for further ongoing collaboration and a model for additional partnerships in the future.
- Providing an interprofessional training experience to 180 medical and 90 nurse practitioner students annually
- Improving attitudes on interprofessional team work pre- vs. post-experience by 10% using a validated scale
- Clarifying aspects of the training experience that promoted or hindered interprofessional teamwork for future partnerships
This program built on a recently developed new competency framework for the medical school, and hoped to respond to evolving accreditations standards around interprofessional education. The program aimed to generate productive learning experiences that could, in addition to transmitting traditional knowledge, provide team activities that shift attitudes, particularly in the domains of: (1) teamwork, roles, and responsibilities; and (2) interprofessional biases. The ultimate goal was to deliver an educational experience that supports provision of patient-, family-, and community-centered care that improves meaningful patient outcomes.
This was the first truly interprofessional learning experience for either training program. While it is sustainable, it fell short of its goals and objectives in key respects. Nevertheless, it created a framework for further ongoing collaboration and a model for additional partnerships in the future.
Structural Dimension:
The original proposal included an interprofessional community experience, which proved logistically challenging. Both Einstein and Columbia students have community experiences woven into their training where they work with other professions (but not the students of other professions). The academic years start in different months, and the Einstein experience is over 4 weeks while the Columbia experience is longitudinal. This kind of hands on experience would seem to be ideal for interprofessional students to learn team roles and responsibilities while addressing biases. However, because of scheduling constraints and logistical hurdles in sharing community placements, this aspect of the program was delayed.
Even without the addition of the community project, broadening the experience to include a wider variety of professions might have improved the experience. We used an existing team-based learning educational experience, which lends itself to sustainability. However, team-based learning, while encouraging students to work as a team, was not explicitly designed to promote role clarification among interprofessional team members, for example. The program as implemented was held at Einstein, which posed travel challenges for Columbia students. It probably would have helped to have at least one session at each campus.
With regard to evaluation, we obtained robust information from attitudinal surveys and focus groups. The main challenge of program assessment was that relevant exam items changed at Einstein over the course of implementation, and there were none for Columbia. This program deepened an existing partnership between professions at two large academic health institutions with varied training programs. Individuals in academic leadership positions were identified and created a partnership. Evaluation and administrative personnel on both sides supported the effort. We did train more than 180 medical students and 90 family nurse practitioner students together each academic year.
The original proposal included an interprofessional community experience, which proved logistically challenging. Both Einstein and Columbia students have community experiences woven into their training where they work with other professions (but not the students of other professions). The academic years start in different months, and the Einstein experience is over 4 weeks while the Columbia experience is longitudinal. This kind of hands on experience would seem to be ideal for interprofessional students to learn team roles and responsibilities while addressing biases. However, because of scheduling constraints and logistical hurdles in sharing community placements, this aspect of the program was delayed.
Even without the addition of the community project, broadening the experience to include a wider variety of professions might have improved the experience. We used an existing team-based learning educational experience, which lends itself to sustainability. However, team-based learning, while encouraging students to work as a team, was not explicitly designed to promote role clarification among interprofessional team members, for example. The program as implemented was held at Einstein, which posed travel challenges for Columbia students. It probably would have helped to have at least one session at each campus.
With regard to evaluation, we obtained robust information from attitudinal surveys and focus groups. The main challenge of program assessment was that relevant exam items changed at Einstein over the course of implementation, and there were none for Columbia. This program deepened an existing partnership between professions at two large academic health institutions with varied training programs. Individuals in academic leadership positions were identified and created a partnership. Evaluation and administrative personnel on both sides supported the effort. We did train more than 180 medical students and 90 family nurse practitioner students together each academic year.
Human Dimensions:
Our faculty members were seasoned at facilitating team learning, but may have benefited from additional training specifically on teaching interprofessional teams. It would probably also have helped to have co-facilitation by faculty from both professions, although this can be logistically challenging. Differences of in-session quiz scores between Einstein and Columbia students suggested that having the material linked to a grade (directly through the quiz, or indirectly through exam material) was important to drive preparation for the sessions. To get meaningful student feedback, incentives were not enough. We needed to piggyback the focus groups on already scheduled activities to make them as accessible as possible.
Our faculty members were seasoned at facilitating team learning, but may have benefited from additional training specifically on teaching interprofessional teams. It would probably also have helped to have co-facilitation by faculty from both professions, although this can be logistically challenging. Differences of in-session quiz scores between Einstein and Columbia students suggested that having the material linked to a grade (directly through the quiz, or indirectly through exam material) was important to drive preparation for the sessions. To get meaningful student feedback, incentives were not enough. We needed to piggyback the focus groups on already scheduled activities to make them as accessible as possible.
Political Dimensions:
Einstein has established interprofessional education as a priority, with multiple pilot projects started with a limited amount of funds available through internal annual grants for excellence in medical education. Aside from the APTR grant, there were no additional funds allocated to this project – it was taken on as part of the duties of the program directors from the two institutions. The leaders from the two institutions had worked together previously and met in person or by phone monthly to formulate and monitor the project. We might have sought broader institutional buy-in to expand to include students from additional professions. The Einstein students were already scheduled for team-based learning, but the Columbia students were accommodating in making this part of their schedule.
Einstein has established interprofessional education as a priority, with multiple pilot projects started with a limited amount of funds available through internal annual grants for excellence in medical education. Aside from the APTR grant, there were no additional funds allocated to this project – it was taken on as part of the duties of the program directors from the two institutions. The leaders from the two institutions had worked together previously and met in person or by phone monthly to formulate and monitor the project. We might have sought broader institutional buy-in to expand to include students from additional professions. The Einstein students were already scheduled for team-based learning, but the Columbia students were accommodating in making this part of their schedule.
Symbolic Dimensions:
Strategically we hoped to use an existing team-based learning experience for Einstein medical students and fold in Columbia family nurse practitioner students to improve attitudes about working in interprofessional teams. We accomplished our goal of implementing the program including our target number of trainees, but our vision of 10% improvement in attitudes based on this modality was not realized. This may provide some lessons learned for those who are considering team-based learning and/or combining these two professions with similar objectives in mind.
Strategically we hoped to use an existing team-based learning experience for Einstein medical students and fold in Columbia family nurse practitioner students to improve attitudes about working in interprofessional teams. We accomplished our goal of implementing the program including our target number of trainees, but our vision of 10% improvement in attitudes based on this modality was not realized. This may provide some lessons learned for those who are considering team-based learning and/or combining these two professions with similar objectives in mind.
IPE OFFERINGS INCLUDE:
- Other: This was a shared experience required for more than 180 Einstein and 90 Columbia students each academic year, but it was 3 two-hour sessions, and not a formal course for credit.
|
PROFESSIONS/DISCIPLINES/SCHOOLS INVOLVED:
|
ACADEMIC LEVELS TARGETED:
|
ASSESSMENT
- Kirkpatrick’s Four‐Levels of Training Evaluation Model (Kirkpatrick & Kirkpatrick, 2006)
- Reaction: Measures how students react to the course; i.e. content and instructional methods
- Learning: Actual learning and acquisition of knowledge
- Behavior: Application of information in structured settings
- Results: Actual changes in clinical practice
|
EVALUATION METHODS DESCRIPTION:
|
EVALUATION METHODS:
|
LESSONS/RESULTS/OUTCOMES
Evaluation Results:
The survey was completed by 59 Einstein and 26 Columbia students. Pooled data for each subdomain showed statistically significant changes in the realms of Patient Centeredness (declined 1.6%; p=0.03 for all students; p=0.01 for Einstein students), Diversity and Ethics (improved 3.8%, p=0.01 for Columbia students), and Community Centeredness (declined 3.0%, p=0.02 for Einstein students; improved 5.0%, p=0.0001 for Columbia students). Aggregate exam scores on related items among Einstein students declined slightly from the pre-intervention to the intervention period, but the number and content of related items on the exam changed somewhat, so direct comparison is difficult. Through a focus group we also wished to assess which aspects of the experience either improved or hindered interprofessional teamwork throughout the experience of both the Einstein and Columbia students. Preliminary analysis of focus group data suggested that students valued the interprofessional learning experience but were not sure the team-based learning modality was the most effective method, with medical students suggesting additional or substitute experiences more closely tied to clinical practice with professions that were less similar in function.
Conclusions
A three-session, 6-hour team-based learning experience across institutions combining medical students in their family medicine clerkship and family nurse practitioner students corresponded with changes in student attitudes. Family nurse practitioner student attitudes in Diversity & Ethics and Community Centeredness improved while medical student attitudes declined around Patient Centeredness and Community Centeredness. It is possible that these changes were due to other experiences, such as the concurrent ambulatory care and community project for medical students, but this is less likely for the nurse practitioner students who were not on a specific rotation during this experience. The two subdomains most explicitly mentioning interprofessional work were unchanged.
The survey was completed by 59 Einstein and 26 Columbia students. Pooled data for each subdomain showed statistically significant changes in the realms of Patient Centeredness (declined 1.6%; p=0.03 for all students; p=0.01 for Einstein students), Diversity and Ethics (improved 3.8%, p=0.01 for Columbia students), and Community Centeredness (declined 3.0%, p=0.02 for Einstein students; improved 5.0%, p=0.0001 for Columbia students). Aggregate exam scores on related items among Einstein students declined slightly from the pre-intervention to the intervention period, but the number and content of related items on the exam changed somewhat, so direct comparison is difficult. Through a focus group we also wished to assess which aspects of the experience either improved or hindered interprofessional teamwork throughout the experience of both the Einstein and Columbia students. Preliminary analysis of focus group data suggested that students valued the interprofessional learning experience but were not sure the team-based learning modality was the most effective method, with medical students suggesting additional or substitute experiences more closely tied to clinical practice with professions that were less similar in function.
Conclusions
A three-session, 6-hour team-based learning experience across institutions combining medical students in their family medicine clerkship and family nurse practitioner students corresponded with changes in student attitudes. Family nurse practitioner student attitudes in Diversity & Ethics and Community Centeredness improved while medical student attitudes declined around Patient Centeredness and Community Centeredness. It is possible that these changes were due to other experiences, such as the concurrent ambulatory care and community project for medical students, but this is less likely for the nurse practitioner students who were not on a specific rotation during this experience. The two subdomains most explicitly mentioning interprofessional work were unchanged.